Toxic Treadmill
Evidence for a Poisoned Planet
Mercury Dental Amalgam Makes Millions Sick
Introduction
Despite over 150 years of warnings, the world is only just waking up to the horrific and cruel practice of putting mercury (Hg) into people's mouths. Authorities, and professionals, have wielded denial, deceit, and ignorance to shield them from responsibility, and liability. Yet, putting one of the most toxic elements known into the mouths of adults and young children alike, has undoubtedly caused significant harm. The likely gravity of such despicable practice brings me to tears, especially knowing that mercury can migrate from a mother to her unborn child during pregnancy. There is no safe level of exposure to elemental mercury.

Mercury in Dentistry: A Century of Warnings Ignored
Dental amalgam is composed of approximately 50% elemental mercury combined with other metals like silver, tin, and copper (all are capable of causing sickness in susceptible individuals). Metal amalgam has been used for well over 150 years. Far from being evidence of safety, this is simply proof of how corrupt, and ignorant, authorities and practitioners have been. Concerns about poisoning from mercury dental amalgam are not new. In 1843, the American Society of Dental Surgeons (ASDS) issued a significant warning of risks of harm from the use of mercury amalgam. They even required their members to sign a pledge not to use mercury-based fillings, describing them as 'malpractice' due to toxicity concerns.
In 1926, German chemist Alfred Stock published a landmark paper describing his own mercury poisoning from amalgam fillings, stating, 'I am convinced that amalgam fillings in the mouth are constantly releasing mercury vapour ... this brings danger to health, in particular to the nervous system.' Stock suffered for decades from severe health issues, including sinusitis. He realized the connection with exposure to mercury vapour after discovering a significant pattern of similar health problems in others who worked with mercury.
I am driven by the fervent desire to warn everyone who has to deal with metallic mercury most emphatically about the dangers of this volatile metal and to spare them the terrible experiences that ruined a large part of my life.
Alfred Stock, 1926.
Clearly, the risk was known. Plus, it's worth remembering that asbestos was in use for over a century before robust action was taken to control its use. Concerns were raised over asbestos as early as the 1890s, due to notable patterns of poor respiratory health in workers. Those concerns were ignored. The same pattern of reckless innovation, and arrogant dismissal of early concern, has occurred with mercury dental amalgam. However, the actual harms caused are likely to be far worse, and meet with even fiercer denial. This pattern has been repeated with novel, gene-based prophylactics, and wireless radiation, too.

How Amalgam Exposure Occurs
Mercury vapour continuously releases from amalgam fillings. It is odourless, invisible, highly lipid soluble, and readily absorbed in the respiratory tract, allowing it to cross the blood-brain barrier and placenta. Levels of release increase during chewing, teeth grinding, brushing, dental procedures, and the consumption of hot liquids. Individual mercury body burden correlates with the number of amalgam fillings. Studies have documented that amalgam bearers exhibit significantly higher mercury levels in various body parts compared to amalgam-free individuals.
Hg accumulates in tissues such as the central nervous system (CNS), liver, and kidneys, and its high affinity for proteins, amino acids, and nucleic acids underpins its toxicity. The way it binds to substances in cells can cause mitochondrial dysfunction; mitochondria power the cells, and are essential for systemic functioning. Mercury vapour is more toxic than its liquid elemental form, and other metals like lead. Autopsy studies indicate that dental amalgams are responsible for 60–95% of mercury deposits in human tissues, highlighting significant bioaccumulation and health risks.
Symptoms and Signs of Mercury Poisoning
Leached mercury can be detected in various biological matrices including urine, saliva, blood, organs, fetal tissues, breast milk, and exhaled air. The body may attempt to excrete it through the skin, hair, or quarantine it in fat stores. Hence, sudden weight loss has potential to release harmful amounts of mercury despite the initial exposure being at an earlier time; months or possibly years beforehand.
Early symptoms of chronic mercury poisoning include weakness, fatigue, anorexia, weight loss, mood perturbation, slow heart rate, and decreasing systolic blood pressure. At higher exposure levels, symptoms extend to severe neuropsychiatric disorder, motor incoordination, and mercurial tremor. Dental personnel exposed to Hg vapour show statistically significant associations between exposure, memory disturbances, and muscular and neuropsychological disorders. The link has been demonstrated in multiple studies across different countries.
Cognitive dysfunctions such as concentration problems, psychosomatic symptoms, and sleep disturbances have also been reported among dental assistants and dentists. Motor performance impairments have been linked to long-term Hg exposure, with noted effects on memory and attention. Signs such as reduced colour vision and abnormal 'visual evoked potentials' (a dysfunction in signalling between the eye and brain) have been observed even at low-level long-term exposure.
Genetic Predisposition and Neurological Harms
Genetic predisposition significantly influences susceptibility to mercury toxicity. Specific gene polymorphisms such as those in brain-derived neurotrophic factor (BDNF), coproporphyrinogen oxidase (CPOX4), catechol-O-methyltransferase (COMT), serotonin transporter (5-HTTLPR), and metallothionein (MT) isoforms (MT1M and MT2A) have been identified to exacerbate neurological and neurobehavioral effects in individuals exposed to mercury from dental amalgam. These genetic variants show additive detrimental effects with mercury exposure, particularly in male children, increasing the risk of neurobehavioural impairments. The damage caused by mercury can lead to excessive anger, depression, prolonged anxiety, impaired memory, and increased suicidal ideation. Such symptoms are often classed and treated as mental illness, such as generalized anxiety disorder, or panic disorder, with no physiological investigation at all.
Research also shows that individual genetic differences influence mercury bioaccumulation and toxic effects. Polymorphisms in genes like GSTM1, GSTT1 (involved in glutathione-mediated detoxification), ABC transporters, metallothioneins, and genes regulating selenoproteins, and xenobiotic transporters, modify mercury metabolism and excretion. For example, GSTT1 gene variants can reduce mercury elimination, increasing retention. Additional studies have identified single nucleotide polymorphisms (SNPs) associated with variations in mercury levels in hair, blood, and urine biomarkers, some related to neurodevelopmental effects.
Mercury exposure impacts gene expression, affecting over 2000 genes including those regulating immune homeostasis, apoptosis, DNA repair, and cellular stress responses. Mercury can cross the blood-brain barrier, and polymorphisms in genes such as APOE (with isoforms APOE2, APOE3, and APOE4) correlate with increased Alzheimer's disease risk when mercury exposure is present.
Large-scale research in Taiwan found that individuals aged 65 and over, with dental amalgam fillings, had a higher risk of Alzheimer's disease compared to those without amalgam exposure. Additionally, a population study of 2 000 subjects in Taiwan indicated that patients with amalgam fillings had a significantly increased risk of Parkinson’s disease. A New Zealand investigation also claimed a connection between amalgam exposure and multiple sclerosis. These data suggest direct links between dental amalgam exposure and neurodegenerative diseases such as Alzheimer’s and Parkinson’s, though this evidence is still emerging and developing.
Genes, Autoimmune Conditions, & Mercury
There is plenty of research connecting mercury exposure to autoimmune disorders. Low-level mercury exposure can disrupt immunoregulatory mechanisms, leading to loss of immune tolerance and autoantibody production. Mercury from dental amalgams has been associated with increased risk for multiple sclerosis, systemic lupus erythematosus, and autoimmune thyroiditis.
Individuals with autoimmune diseases show heightened sensitivity and inflammatory responses to Hg released from dental amalgam, including elevated pro-inflammatory biomarkers like interleukin-8, normalizing after amalgam removal. While immune responses to Hg exposure exist, some immune effects are also likely to be caused, or exacerbated, by the other metals present in amalgams. This gene-environment interaction highlights the complexity of Hg toxicity and the variable individual response based on genetic makeup.
Synergistic Effects with Other Toxins
Mercury from dental amalgam acts synergistically with other environmental toxins, creating a 'total body burden' effect. Even low-level mercury exposure, when combined with other heavy metals like lead or cadmium, produces neurotoxic effects at levels where exposure to mercury alone would show no measurable impact.
Besides cadmium, dental mercury also interacts with aluminium, arsenic, and organophosphates (commonly found in food and the environment). This amplifies oxidative stress and cellular damage. However, the complexity of synergistic effects, and the failure to consider them in safety assessments, means that such scientific research has received grossly inadequate attention or funding.
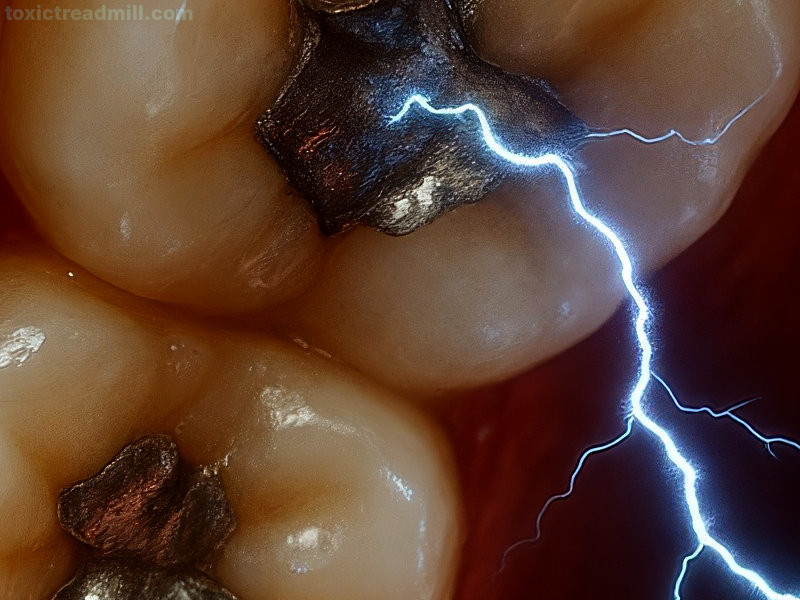
Dental Metal, Galvanic Currents, Non-ionising Wireless Radiation, & Pathophysiology
Galvanic currents are direct currents caused by a flow of electrons. The mouth is particularly susceptible to electric flows because it is wet. Humans are electrical in nature with many processes governed by ion flows, charge orientation, and electric pulses. Introducing metallic elements of any kind can introduce novel galvanic currents. Little mention is made of these in reference to mercury-based dental amalgam, but research shows such interference may cause detrimental physical effects, including cytotoxicity. Galvanosis is a known condition caused by electrical currents generated within the mouth due to the interaction of different metals. These currents can lead to discomfort, burning sensations, and potentially, more serious oral health problems. There may also be a causative association with nasal diseases, including rhinitis. Increased release of mercury from amalgam, and nickel from orthodontic appliances, has been found when exposed to RF radiation (similar to that used in mobile phones and other domestic Wi_Fi appliances) in laboratory conditions, which further compounds the issue.
Fraud, Adulteration, and Contamination Concerns
As with every other area of commerce, there are troubling patterns in amalgam production and marketing. Some manufacturers fail to disclose full ingredients or knowingly misrepresent safety data, particularly regarding mercury vapour release rates. Analysis of amalgam products has revealed that a number contain undisclosed metals and higher-than-reported mercury content. Such adulteration can lead to increased toxicity and unexpected allergic reactions. There have also been concerns over batch-to-batch variation in amalgam composition from several manufacturers, raising questions about product consistency and safety assurance.
Removal, Detoxification, and Recovery
Hg levels in urine and blood tend to decrease rapidly after exposure cessation, but Hg accumulates in organs with half-lives of several years, indicating lasting effects. Importantly, meta-analyses have shown persistent neurological effects even after exposure stops, with critical urinary Hg levels identified around 300 nmol Hg/L, though effects have been noted below this level. Even after all mercury amalgam has been removed, it can take anywhere from several weeks to a decade or more for the body to detoxify, depending on the individual physiology and the extent of contamination. Both repair and removal require careful management, including use of a dam, vacuum removal of loose pieces, and continuous vacuum extraction of vapours.
Chelating agents are sometimes recommended. These are intended to bind loose mercury and help flush it out of the body. However, the complexity of biological systems, and propensity for binding non-mercury metallic elements that the body requires, make this a complicated consideration. Similarly, supplementing with displaced nutrients, such as selenium, zinc, and calcium might help restore function as the mercury is flushed, but this also depends on diet, individual physiology, and other health conditions. There is no guarantee of partial or complete recovery. Significant rest and a prolonged period of reduced stress will assist. However, some symptoms and diseases, especially those linked to epigenetic changes or damaged organs, will be irreversible.
Global Regulatory Status
The Minamata Convention
The Minamata Convention on Mercury, signed in 2013, and which came into effect in 2017, requires participating nations to phase down their use of mercury. As of 2024, 128 countries have ratified the convention. The convention explicitly addresses dental amalgam and requires that dental amalgam should NOT be used in deciduous teeth, in children under 15, or in pregnant or breastfeeding women.
National Bans on Dental Mercury
- Canada prohibited the use of mercury amalgam in temporary teeth in 1993, and followed up in 1995, by banning its use in anyone under 19.
- Sweden began a phased ban in 1994, and was the first country to completely ban dental amalgam in 2009 with limited exceptions which were removed in 2018
- Norway banned its use in 2008 based on environmental concerns
- Denmark restricted its use in 1995
- Finland phased out all amalgam use in 2019
Notably, Sweden, Norway, Denmark, and Finland have consistently better health index scores than the UK. Many other countries have already imposed restrictions on the use of dental mercury including EU members who are obliged to adopt the 2018 European Union ban for children under 15, pregnant or breastfeeding women, and a total ban was implemented at the beginning of 2025 with limited exceptions which will expire in 2026. This ban not only prevents the use of dental mercury, but also its manufacture, import, and export.
The UK has implemented some restrictions, but the aspiration to improve the health of the nation continues to languish far behind counterproductive motivation for the fulfilment of material desire. An obnoxious and ignorant stance maintained by the British Dental Association, and an NHS policy favouring mercury use, have long inhibited professionals from improving their knowledge of the harms of mercury amalgam, and upskilling in the use of alternatives. Britain's traditional 'cartel of carelessness', a loose affiliation of glib, self-serving politicians, and supercilious industry representatives, continues at the expense of the health and wellbeing of the population.
The BDA continues to evade facing the horrors of harm it has caused. Mercury amalgam bans are often reframed as being necessary for environmental concerns, with continued claims that they are safe to put into your mouth. We are supposed to accept that amalgam is harmless, and does not release mercury, despite having surfaces directly exposed to hard grinding friction, sticky suction, temperatures from zero to 50+ Celsius, multiple organic and synthetic compounds, and a pH range anywhere from 2 (lemon juice) to 10+ (chewable antacid tablets), several times a day, over decades. Additionally, the risk from amalgam coming loose and being swallowed, a fairly common occurrence among toffee-chewing kids, seems to be ignored completely. Yet, the moment this 'harmless' substance is removed from your mouth, it suddenly becomes a biohazard that legally requires specialist disposal, with failure carrying the threat of criminal prosecution. This level of absurdity is difficult to match, even in the historical claims made by the tobacco industry.
References
Baek, H. J., Kim, E. K., Lee, S. G., Jeong, S. H., Sakong, J., Merchant, A. T., ... & Choi, Y. H. (2016). Dental amalgam exposure can elevate urinary mercury concentrations in children. International Dental Journal, 66(3), 136-143.
Basu, N., Bastiansz, A., Dórea, J. G., Fujimura, M., Horvat, M., Shroff, E., ... & Zastenskaya, I. (2023). Our evolved understanding of the human health risks of mercury. Ambio, 52(5), 877-896.
Bjørklund, G., Dadar, M., Chirumbolo, S., Aaseth, J., & Peana, M. (2020). Metals, autoimmunity, and neuroendocrinology: Is there a connection?. Environmental research, 187, 109541.
Bjørklund, G., Peana, M., Dadar, M., Chirumbolo, S., Aaseth, J., & Martins, N. (2020). Mercury-induced autoimmunity: drifting from micro to macro concerns on autoimmune disorders. Clinical immunology, 213, 108352.
Bjørklund, G., Tinkov, A. A., Dadar, M., Rahman, M. M., Chirumbolo, S., Skalny, A. V., ... & Aaseth, J. (2019). Insights into the potential role of mercury in Alzheimer’s disease. Journal of Molecular Neuroscience, 67, 511-533.
Björkman, L., Musial, F., Alræk, T., Werner, E. L., Weidenhammer, W., & Hamre, H. J. (2020). Removal of dental amalgam restorations in patients with health complaints attributed to amalgam: a prospective cohort study. Journal of Oral Rehabilitation, 47(11), 1422-1434.
Cabaña-Muñoz, M. E., Parmigiani-Izquierdo, J. M., Bravo-González, L. A., Kyung, H. M., & Merino, J. J. (2015). Increased Zn/glutathione levels and higher superoxide dismutase-1 activity as biomarkers of oxidative stress in women with long-term dental amalgam fillings: correlation between mercury/aluminium levels (in Hair) and antioxidant systems in plasma. Plos one, 10(6), e0126339.
Chepelova, N., Antoshin, A., Voloshin, S., Usanova, A., Efremov, Y., Makeeva, M., ... & Timashev, P. (2023). Oral Galvanism Side Effects: Comparing Alloy Ions and Galvanic Current Effects on the Mucosa-like Model. Journal of Functional Biomaterials, 14(12), 564.
Emeny, R. T., Korrick, S. A., Li, Z., Nadeau, K., Madan, J., Jackson, B., ... & Karagas, M. R. (2019). Prenatal exposure to mercury in relation to infant infections and respiratory symptoms in the New Hampshire Birth Cohort Study. Environmental research, 171, 523-529.
Geier, D. A., & Geier, M. R. (2021). Dental amalgams and the incidence rate of arthritis among American adults. Clinical Medicine Insights: Arthritis and Musculoskeletal Disorders, 14, 11795441211016261.
Golding, J., Steer, C. D., Gregory, S., Lowery, T., Hibbeln, J. R., & Taylor, C. M. (2016). Dental associations with blood mercury in pregnant women. Community dentistry and oral epidemiology, 44(3), 216-222.
Hsu, Y. C., Chang, C. W., Lee, H. L., Chuang, C. C., Chiu, H. C., Li, W. Y., ... & Fu, E. (2016). Association between history of dental amalgam fillings and risk of Parkinson’s disease: a population-based retrospective cohort study in Taiwan. PloS one, 11(12), e0166552.
Jafari, T., Rostampour, N., Fallah, A. A., & Hesami, A. (2017). The association between mercury levels and autism spectrum disorders: a systematic review and meta-analysis. Journal of Trace Elements in Medicine and Biology, 44, 289-297.
Jirau-Colón, H., González-Parrilla, L., Martinez-Jiménez, J., Adam, W., & Jiménez-Velez, B. (2019). Rethinking the dental amalgam dilemma: an integrated toxicological approach. International journal of environmental research and public health, 16(6), 1036.
Just, A., & Kall, J., DM. (2017, June 15). Why we all don’t get sick in the same way: The science behind dental mercury and other environmental toxicants. International Academy of Oral Medicine and Toxicology.
Kall, J., Just, A., & Aschner, M. (2016). What is the risk? Dental amalgam, mercury exposure, and human health risks throughout the life span. Epigenetics, the environment, and children’s health across lifespans, 159-206.
Khan, F., Momtaz, S., & Abdollahi, M. (2019). The relationship between mercury exposure and epigenetic alterations regarding human health, risk assessment and diagnostic strategies. Journal of Trace Elements in Medicine and Biology, 52, 37-47.
Kristoffersen, A. E., Alræk, T., Stub, T., Hamre, H. J., Björkman, L., & Musial, F. (2016). Health complaints attributed to dental amalgam: a retrospective survey exploring perceived health changes related to amalgam removal. The Open Dentistry Journal, 10, 739.
Llop, S., Ballester, F., & Broberg, K. (2015). Effect of gene-mercury interactions on mercury toxicokinetics and neurotoxicity. Current environmental health reports, 2, 179-194.
Maqbool, F., Niaz, K., Hassan, F. I., Khan, F., & Abdollahi, M. (2017). Immunotoxicity of mercury: Pathological and toxicological effects. Journal of Environmental Science and Health, Part C, 35(1), 29-46.
Morris, G., Puri, B. K., Frye, R. E., & Maes, M. (2018). The putative role of environmental mercury in the pathogenesis and pathophysiology of autism spectrum disorders and subtypes. Molecular neurobiology, 55(6), 4834-4856.
Mortazavi, G., & Mortazavi, S. M. J. (2015). Increased mercury release from dental amalgam restorations after exposure to electromagnetic fields as a potential hazard for hypersensitive people and pregnant women. Reviews on environmental health, 30(4), 287-292.
Mortazavi, S. M. J., Paknahad, M., Khaleghi, I., & Eghlidospour, M. (2018). Effect of radiofrequency electromagnetic fields (RF-EMFS) from mobile phones on nickel release from orthodontic brackets: An in vitro study. International orthodontics, 16(3), 562-570.
Navas-Soler, B., Palazó, A., Vallejo-Ortega, J., Santano-Pé, C., Seguí, C., Seguí, M., ... & Seguí, M. (2025). Multiple Chemical Sensitivity: A Sickness of Suffering, Not of Dying. Descriptive Study of 33 Cases. Health, 17(1), 65-81.
Paknahad, M., Mortazavi, S. M. J., Shahidi, S., Mortazavi, G., & Haghani, M. (2016). Effect of radiofrequency radiation from Wi-Fi devices on mercury release from amalgam restorations. Journal of Environmental Health Science and Engineering, 14, 1-6.
Pamphlett, R., & Kum Jew, S. (2019). Mercury is taken up selectively by cells involved in joint, bone, and connective tissue disorders. Frontiers in Medicine, 6, 168.
Parajuli, R. P., Goodrich, J. M., Chou, H. N., Gruninger, S. E., Dolinoy, D. C., Franzblau, A., & Basu, N. (2016). Genetic polymorphisms are associated with hair, blood, and urine mercury levels in the American Dental Association (ADA) study participants. Environmental research, 149, 247-258.
Rahbar, M. H., Samms-Vaughan, M., Saroukhani, S., Bressler, J., Hessabi, M., Grove, M. L., ... & McLaughlin, W. (2021). Associations of metabolic genes (GSTT1, GSTP1, GSTM1) and blood mercury concentrations differ in Jamaican children with and without autism spectrum disorder. International journal of environmental research and public health, 18(4), 1377.
Roy, C., Tremblay, P. Y., & Ayotte, P. (2017). Is mercury exposure causing diabetes, metabolic syndrome and insulin resistance? A systematic review of the literature. Environmental research, 156, 747-760.
Stejskal, V., Reynolds, T., & Bjørklund, G. (2015). Increased frequency of delayed type hypersensitivity to metals in patients with connective tissue disease. Journal of Trace Elements in Medicine and Biology, 31, 230-236.
Stock, A. (1926). Die gefährlichkeit des Quecksilberdampfes. Angewandte Chemie, 39(15), pp.461-466.
Sutow, E. J., Maillet, W. A., Taylor, J. C., & Hall, G. C. (2004). In vivo galvanic currents of intermittently contacting dental amalgam and other metallic restorations. Dental Materials, 20(9), 823-831.
Vankar, P. (2024, February 24). Health and health systems ranking of European countries in 2023, by health index score. Statista. Retrieved May 8, 2025, from https://www.statista.com/statistics/1376355/health-index-of-countries-in-europe/
Vieira, A. R., Silva, M. B., Souza, K. K., Filho, A. V., Rosenblatt, A., & Modesto, A. (2017). A pragmatic study shows failure of dental composite fillings is genetically determined: a contribution to the discussion on dental amalgams. Frontiers in medicine, 4, 186.
World Health Organization. (2017). Mercury and health fact sheet. World Health Organization: Geneva, Switzerland, 31.